Having children was always something my husband and I had looked forward to. We would often imagine what our future family would be like. My husband had unfortunately lost his only brother at the age of 31, so had always expressed his desire to have at least 3 children. I come from a large extended family so felt I would rather have 4 children than 3. In 2005 after two and a half years of trying to conceive and one miscarriage we finally conceived, and our journey as parents began……
At 32 weeks pregnant I had noticed lack of foetal movement and my instincts felt that something wasn’t right. I went to triage and was monitored for the next 24 hours. Decelerations were apparent and they gradually became more frequent, eventually signalling that the baby was in distress. One minute I was sitting eating lunch and the next I was having an emergency caesarean section (EMCS). Our son was born and resuscitated on delivery. He was then admitted to neonatal intensive care unit (NICU) and I wasn’t able to see him for 24 hours. It was all very rushed and I remained in shock. This was not how I had imagined my transition into parenthood to be? I was however grateful that my son was alive and apparently beautiful. I was yet to meet him…
When my son was 5 months old I discovered I was pregnant again, although we hadn’t planned this pregnancy we both felt blessed. At 24 weeks I had a bleed followed by several more. I was diagnosed with having placenta previa grade 4. This was a very hard time for us and my husband had to take time from working to care for my son and me. I was under strict instructions not to lift or do anything other than sit and rest because of the risk of haemorrhage. It was expressed that this could potentially be life threatening. I was also diagnosed with gestational diabetes so had to maintain a restricted diet. Eventually following another bleed, at 33 weeks I was admitted to hospital on full bed rest until the baby arrived. I felt so depressed and being parted from my first son made me very emotional. I was in hospital for his first birthday whilst my family celebrated. Inside I feared that I would not bond with my baby as I was already resenting him for the situation I found myself in. I just wanted to make it through this pregnancy and return to being a mom to my child.
At 37 weeks I haemorrhaged and it was scary. I sat on the toilet whilst the blood poured down my legs. I pulled the emergency cord and I felt grateful to be in hospital. The reality of this scenario was something that I had totally underestimated. I signed the consent form to have a hysterectomy and was rushed into theatre for a crash section under general aesthetic. I can remember my body violently shaking whilst lying on the cold operating table. The medics were rushing around getting blood into me and preparing me for surgery. I knew nothing more as I had blacked out……. When I woke I had drips attached and bloods being administered along with a catheter and a Bakri balloon inserted, to stop the internal bleeding. Although I lay there helpless and vulnerable I was grateful for mine and my son’s life. There was also the added bonus of my uterus still contained inside of me. I lay looking at my son in his crib wishing to cradle him and celebrate that we had made it through a very tough time, but I couldn’t move. I loved him so much and couldn’t believe I ever doubted that I would. I needed to recover and gain strength so I could care for my family again.
The years went by and as much as we both wanted more children, we were both fearful of what another pregnancy may bring. Eventually, 7 years after my last baby we decided to try for another baby. I was fortunate enough to fall pregnant quite soon. At my booking appointment I was categorised as being “high risk” so it was explained that my care would be consultant led. I asked if I could have a natural birth this time but was told no and that it was not allowed after 2 c sections. Being unsure of how the pregnancy would unfold I didn’t contemplate questioning this decision. I had accepted the decisions made by others regarding my care and my birth and wasn’t aware that there were any alternatives. The months went by and I felt fantastic! I was screened for gestational diabetes and the result was negative. My scans had shown that my placenta was not covering my cervix. My baby was growing perfectly and I was still attending a kickboxing exercise class at 5 months pregnant.
My 36/37 week appointment with my consultant was approaching. I had understood that at this appointment my caesarean section would be discussed. The thought of surgery and my memories of my previous experiences including recovery depressed me. I felt too well and healthy to end this pregnancy in surgery.
My appointment was in three days and whilst browsing on the internet I typed “natural birth after 2 caesareans”. I was so excited by what I found. I became engrossed in a world that I never knew existed, the world of vaginal birth after 2 caesareans (VBA2C)…. I joined forums and spoke to women in my situation; I read guidelines applicable to my situation. I also read the risks involved with a third c section and the implications of those risks on a fourth pregnancy. The more knowledge I gathered the more I believed I was a suitable candidate for a VBA2C. My mum had given birth and had been asked to give talks on her breathing techniques. My sister had given birth 3 times, one of them being a homebirth to which I had witnessed. I began to question why I was to undergo major abdominal surgery for no apparent medical reason other than the fact I had had 2 previous caesarean sections? I then began to wonder why all this information was not discussed with me by those that were responsible for my care. Maybe it was because I had not actually met my consultant yet and only met various different members of his team.
I called ahead of my appointment and expressed that I wanted to meet my consultant and discuss the possibility of a vbac. I felt that by speaking to the most senior member of the team I would have the opportunity to discuss all of my options in depth and could compare the rationale behind each mode of delivery. I would respect their opinion as they would know best? I was told that he was not available and that I would need to see his registrar. I didn’t feel happy with this so tried to arrange an appointment with my previous consultant that was also based at my hospital. This was not possible so I accepted the appointment with the registrar. When I met with the registrar, I explained that I had been looking at the possibility of vaginal birth after caesarean (VBAC) versus another C-section and explained to her some of my reasons for wanting a VBAC.
• Risk of infection.
• Difficultly looking after 3 children after having major abdominal surgery.
• Risk associated with 4 pregnancies after 3rd c section, i.e. placenta previa/ accreta.
• My children seeing me looking poorly.
• Higher chance of NICU admission.
• Risk of respiratory problems.
• Higher chance of hysterectomy.
• Scarring and adhesions.
The main risk I could find associated with a vaginal birth was risk of rupture at 0.8%, This figure also included those labours that were augmented and the catastrophic risk included in this statistic was in fact much smaller. I felt that the benefits of a vaginal birth being successful were huge. So that meant a 99.2% that a rupture would not occur? This statistic of 99.2% seemed to me to be better than those associated with elective caesarean section (ELCS).
I was met with a negative response. I was told I could definitely not have a VBAC and that I was ridiculous to suggest it. During our conversation the registrar emphasised the risk and catastrophe I would be facing if I were to attempt a VBAC. Only some of her comments are listed below
.
• VBAC was not an option, C section was a must.
• 80 % chance of uterine rupture.
• Why think about fourth pregnancy just focus on the current one.
• I had never dilated and wasn’t sure if I could do so, so would not risk me labouring.
• I would not find “anyone” that would support me.
• In her previous employment she had met someone like me and that no one wanted them on their watch!!!!
• If I went into labour naturally I would automatically be taken in for EMCS. Trail of labour after caesarean (TOLAC) was not an option.
I then explained that I had researched the Royal College of Obstetricians and Gynaecologist (RCOG) guidelines and National Institute for Health and Care Excellence (NICE) guidelines and that was my grounds for believing I was a suitable candidate and that vba2c was a safe option. I asked if she knew of the guidelines I was referring to? She then explained that she wasn’t as she didn’t have time to go on computers much?? I asked her to access them on her computer whilst I was present. She displayed the guidelines on her computer and began reading. She expressed that they were applicable to 1 previous c section and did not apply to my situation. I then highlighted the relevant section within the guidelines.
RCOG guidelines
“Women with a prior history of two uncomplicated low transverse caesarean sections, in an otherwise uncomplicated pregnancy at term, with no contraindication for vaginal birth, who have been fully informed by a consultant obstetrician, may be considered suitable for planned VBAC.”
NICE quality standards states
“Clinically there is little or no difference in the risk associated with a planned caesarean section and a planned vaginal birth in women who have had up to 4 previous caesarean sections. If a woman chooses to plan a vaginal birth after she has previously given birth by caesarean section, she should be fully supported in her choice.”
I requested that she print them off so I could keep them alongside my handheld notes. She then left the room to retrieve the documents from the printer. My husband and I sat in the room for what felt like eternity. My husband then began questioning my motives and the validity of the information I was quoting. He felt that they should know what they were talking about; after all they were the professionals. I asked him to be quite and leave me to do the talking.
The registrar then returned holding the guidelines and was accompanied by a man that turned out to be my consultant; the one that was originally supposed to be on leave therefore was unavailable for my appointment? He introduced himself and acknowledged my request for a vba2c and the fact that I was aware of the applicable guidelines. He then began to explain that although the guidelines were in place, very few obstetricians agreed with them or felt happy caring for a woman that wanted to attempt a vbac after more than 1 c section: He explained that it was important that we both felt happy with the chosen method of birth and suggested that I go away and discuss this with my husband and to take more time to consider my options. He wanted me to take into account the following:
• Although the guidelines were in place, very few obstetricians felt comfortable with a woman attempting a VBAC after 2 or more c sections.
• If I were to rupture it is catastrophic.
• I could be that catastrophe and he wouldn’t want his name associated with that.
He asked my husband, “What was more important…? A natural birth or me being a mother to my other children??? “
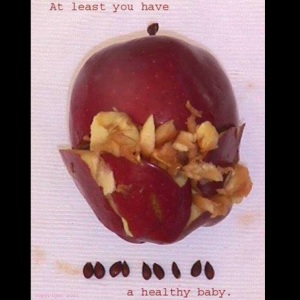
Neither the consultant nor the registrar had looked at my medical history or referenced my notes to support their decisions. We got up to leave and the registrars parting words were said through smiles, “I have booked your c section so you don’t miss your spot and labour ward will be in contact with the date.” I left the building in turmoil! My face was bright red, my eyes were blood shot and I felt shaky inside. My husband began to side with the doctors and said he thinks it’s better if I just have a caesarean as he didn’t want to lose me, he felt it was just not worth it and that the doctors were the professionals and therefore knew what was for the best. He agreed with them that the most important thing was that I was alive and well to parent my children. This was something that I would never jeopardise. My children were my driving force at all times. He then went on to explain that he thinks they thought I had fallen from a tree and banged my head, implying that they thought I was mad judging by the way they had spoke to me. I had nothing left inside so I just remained quite.
I got home and I found my big blanket and buried myself on the sofa underneath for protection. I felt scared, vulnerable and disempowered. I had been told that if were to go into labour I would be taken straight into theatre for surgery. To me that felt threatening and left me fearful. I remained on the sofa for the rest of the evening not interacting with my children as I felt void and numb. Maybe I was going mad?
I woke the next morning, grateful for a fresh new day. I sat drinking my tea evaluating the consultant meeting. I began to feel concerned. Was the care that I was receiving evidence based? What happened to informed consent? Was I being coerced into surgery? Were my best interests at the centre of those responsible for my cares’ decisions? I decided to get a second opinion from someone outside of my hospital. After all it had been pointed out that they were all of the same opinion and that no one would support me.
I managed to contact the Local Supervising Authority Midwifery Officer (LSAMO) and spoke to a lady called Kate Brintworth. I explained my desire to have a VBA2C and the reasoning behind my decision. I explained the options I was facing and how that left me feeling. Kate expressed that she was concerned that I was feeling vulnerable and that I was now approaching 38 weeks with no birth plan in place. She would arrange to put me in contact with Cathy Walton, the Consultant midwife for Kings College Hospital, for some support and that I would have an opportunity to explore my options. She also reassured me that I wasn’t going mad and that my requests were valid. On the Wednesday Cathy Walton called and listened to my concerns. She offered to be a mediator and would liaise with those responsible for my care with a view to arranging another meeting hoping that the outcome would be more reassuring. Cathy had spoken to the clinical lead and the Supervisor of Midwives (SOM) and had reassured me that they would be in touch. Cathy had expressed that she was there if I needed her in the meantime. Cathy’s’ offer of support made me feel safer and stronger.
By Thursday evening I called the SOM as I hadn’t yet had a response. She explained that she hadn’t accessed my notes so could not discuss it any further and would contact me when she had done so. Friday came and so I called again as I was feeling anxious that the weekend was approaching and here I was approaching 38 weeks pregnant and still had no new options or a birth plan in place. Once again the SOM said she hadn’t had time to look at my notes and that she was extremely busy. By now I was very concerned at the way I was being treated and my confidence in their ability to care for me was dwindling. I was concerned that I may go into labour over the weekend so I decided that I would write a letter and hand deliver it in order to try and gain some control over my care and my body. I addressed the letter to the Chief executive, my consultant, the SOM and what I believed was the Head of Midwifery. Some Extracts from the letter are listed below.
• “Unless there are any medical contraindications that occurred during my previous C section’s that will impact on the success of a VBA2C, I will not be pursuing an elective Caesarean section.”
• “I would therefore like you to put any necessary arrangements in place to support and assist me with this. Please could you confirm in writing that you have done so?”
• “I am hoping this meeting will be less stressful and will take place on Monday, as I will be over 37 weeks pregnant with no birth plan in place.”
• “Should you feel that there is medical reason to prevent me having a VBAC please notify me ASAP.
Also if you feel you are unable to provide the support I need please also notify me ASAP.” I would not willingly allow anyone to carry out major abdominal surgery for no apparent medical reason. Surely that alone posed a major risk?
At 7 pm that evening the SOM left a message on my answering machine to say she would call me on Monday to arrange an appointment for later that week. I spent the weekend lying on the sofa scared to move in case I provoked labour. I had never experienced any form of labour, nor had I any antenatal classes so did not know what to expect or signs to look for. By Monday afternoon I still hadn’t heard from my hospital so I called Cathy Walton and asked if I could see a consultant at Kings College Hospital. I wanted an opinion that was based on my medical history and relevant evidence. It was really important for me to know if there was a medical reason for a repeat caesarean.
An appointment was made for the following day. I prepared myself for the battle that believed I was about to face. I sat with the new consultant and explained my reasoning for my wanting a VBA2C and my belief that I was a suitable candidate. To my utter disbelief the consultant had accessed my medical history and she stated the following:
• She felt I was fully informed.
• Aware of associated risks of c/section and VBAC.
• A successful VBAC was the safest option pending future pregnancy.
• No medical reason to prevent VBAC as an option.
• Fully supportive of VBAC pending scan and position of my placenta.
I had worked myself up for nothing? I sat in the room with Cathy and the consultant and I cried! Here I was with not 1 but 2 ladies that supported my birth choice. The fear and the worry rolled down my face and away from my mind in the form of tears. I began to relax and feel safe. The next day I had the scan and my placenta was in a good location for a vaginal birth.
Still not having heard anything from my hospital, at 38 weeks I decided to transfer my care and start preparing to give birth. Part of the care I had agreed to involved me having sweeps from 39 weeks to maximise my chance of going into spontaneous labour. I hadn’t researched this type of intervention and went along with it. At exactly 40 weeks I noticed I had some pink discharge and some watery looking blood. Never having been in this situation before I wondered if this was a sign of rupture? I went to Triage and after examination it was confirmed that my waters were leaking. It was suggested that I could go home and hopefully I would start contracting and that labour would begin. I agreed to return to the labour ward the following day. I went home a prayed for my labour to start, but unfortunately nothing happened.
I returned to labour ward the following day and the doctor in charge suggested that as it was approaching 48 hours of my waters leaking he could examine me and if my waters were intact he would artificially rupture my membranes (ARM) with a view to start labour and that if nothing had happened in 2 hours they would perform a c section… I explained that I wasn’t happy with this suggestion and refused an examination. I asked if there were alternative options? He then explained that as mine and the babies observations were good I could go home and hope labour would start. He asked me to take some pre operative medication and to fast from 7pm that evening and return for surgery at 9 am the next day. I got home and I sat and looked at the pre op medication and I felt defeated! Taking this medication was like submitting to surgery. I then reflected over my previous surgeries and reasoned that they had both been performed immediately after meals. With that in mind I decided I was not going to take this medication as I was not giving up hope just yet. I also felt that fasting wasn’t good as I believed I needed all the energy I could get if I were to go into labour and I believed I would.
I decided I was going to try everything within my power to start labour. I called an acupuncturist and she came to my house and gave me a course of acupuncture so strong that it caused involuntary movements. I ordered an Indian and thoroughly enjoyed eating it. I walked nearly 10k. I used my breast pump for nipple stimulation. I drank the juice of 8 pineapples and I had my friend round and we laughed and joked. I went to bed at 11pm exhausted but feeling at peace that what was going to be would be and it was now down to nature.
I woke at 7am having had the best night’s sleep ever! I hadn’t even woken to go to the toilet? Perhaps that was the reason that urine was trickling down my legs as I made my way to the bathroom? It was in fact my waters and at 7.06am on Sunday morning at 40+3 my contractions began! At 10 am I called the labour ward and explained that I was in labour and that I would stay at home until I felt the time was right to come in. I enjoyed this feeling of being in labour. I felt so lucky that here I was swaying rhythmically as the contractions waved through my body. I was going to embrace this experience. I ate throughout the day and I laboured with my children by my side whilst I rocked on my birthing ball. I walked around my house as my mum mopped the liquor that was flowing from me with each contraction. As I embraced these feelings I began to feel stronger with each contraction. By 4pm that afternoon my mum was expressing that she thought I should be in the hospital as she was envisioning delivering the baby. I was trying to hide my discomfort from my children so I agreed.
I was examined on arrival at the hospital, I was 4cm dilated and my fore waters were still intact. I was surprised as I had been losing so much fluid. I joked that I may give birth to a tadpole? The same doctor that I had seen the day before came bounding into my room full of smiles. He explained that it was good news that I was 4cm and was in labour and that as my waters were bulging but intact. He then suggested that he would break them and speed up labour due to risk of infection?? If the baby is not born in 2 hours he would carry out a c section? It was then that I politely but firmly said that I had no intention of having a caesarean, especially not in fear of risk of infection that myself and the baby were showing no signs of? The risk of infection due to surgery amongst other risks was of a greater concern to me. I explained whilst swaying side to side with contractions that here I was in labour and what a big achievement that this was for me. I expressed that I intended to let the labour take its course. I made it quite clear that I would only consider a caesarean if it was a true medical emergency and that mine or my baby’s’ life were being compromised. I then asked him to leave the room so I could continue to labour and stated that doctors were no longer permitted to enter, except in the case of an emergency.
I then continued to labour on the floor, on my knees remaining as active as possible and taking regular trips to the toilet. I refused all pain relief as I feared that I would lose control leading to interventions. I just requested Paracetamol and used gas an air when needed. My baby was OP and I found that leaning forward helped to relieve the pain in my back. I found myself in a trance like state and could not contemplate talking to anyone. I remember questioning in my thoughts how women could use their energy to shout out? The act of childbirth and all that was happening to my body consumed and silenced me. I began to feel the urge to push at around 4am the following day. The midwives felt it was not time yet but my body was taking over. I surrendered to these feelings as my physical being took charge. I began to push and 10 minutes later my beautiful son was born! I had just experienced the most amazing thing ever! I had given birth!
There is no other experience that can compare to this.
I felt physically and emotionally strong. My maternal being was in full force and I now felt complete as a woman. I had finally put Mother Nature’s gift to the test and it proved to be everything I had hoped for and so much more.
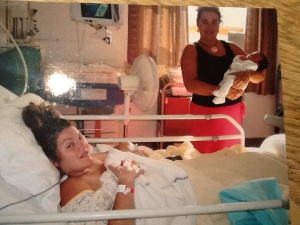
I finally get to hold my baby. No drips, catheters or balloons. Up and walking the same day.
MRS INDEPENDANT!!
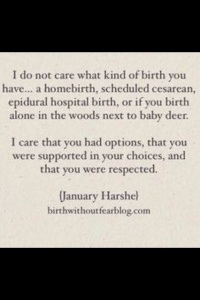
Mother Nature’s Gift
A Women’s ability to give birth is miraculous. Every woman has the right to experience this if they choose and if it is possible.
I wanted to experience my body doing what it was made to do.
No woman should be denied and prevented from giving birth because of another person’s subjective views and fears.
My final thought
BY
Michelle Quashie





 After two previous traumatic Caesarean sections, followed by a hospital vba2c, my home birth was everything I have learnt that birth can be.
After two previous traumatic Caesarean sections, followed by a hospital vba2c, my home birth was everything I have learnt that birth can be.